Vertigo – The Theory of Planned Behavior: A Patient’s Control Dilemma
- The Theory of Planned Behavior (TPB) goes beyond the purely rational, “expectancy–value” approach to examine other elements of decision-making.
- TPB can help practitioners predict patient behavior and address concerns that they otherwise might not express.
- The TPB includes both social considerations and questions of the patient’s control over their condition.
How do people make difficult decisions?
How do people decide which career to undertake, what car to buy, or whether to take medication? Important decisions are typically the result of some degree of thought and planning, a process that Daniel Kahneman labelled “System 2” thinking in his groundbreaking book, Thinking Fast and Slow.1 What is the mechanism people use to reach conclusions?
For many years, decision making was largely considered to be a process driven by “expectancy–value” considerations, the sort of cost-benefit analyses most are familiar with: “I will gain X from doing that, but it will cost me Y in terms of money, effort, or time.” If X is perceived to be greater than Y, people will execute the decision.
The Health Belief Model, which was examined in the last article in this series, << Understanding Patient Attitudes: The Health Belief Model >>, is this type of expectancy–value model, applied to health behavior. However, people are not purely rational, and other factors beyond purely rational considerations are often included in the decision-making process.
External considerations
In the 1980s, Icek Ajzen and others crafted a model to help incorporate factors into the purely rational expectancy-value models that had dominated behavioral theory until then.2 He pointed out that people have different attitudes or beliefs about given behaviors, and, as social beings, those attitudes and beliefs can be influenced by others. The opinions of others, e.g. family, friends, and even society as a whole, about a behavior may be included as an influencing factor on individual decisions. Smoking habits are a good example; while people smoke for a variety of reasons, sometimes one of those reasons is simply a desire to conform to or confound the opinions of those around them.
The Theory of Planned Behavior (TPB)
The Theory of Planned Behavior puts these considerations together in a model to understand and predict behavior:
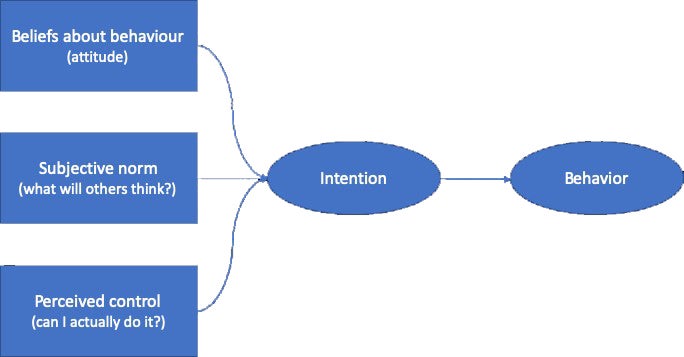
The TPB suggests that people will at least form the intention to carry out a given behavior if all three of the domains – beliefs about a behavior, the perception of a subjective norm, and the perception of control – come together as shown in the diagram above. Factors that may appear irrational are discussed here; however, other considerations may still prevent the desired actions from taking place. For example, a lack of opportunity or lack of ability to act may prevent intention from becoming behavior; such “process” interruptions will be investigated in future articles.
What does the Theory of Planned Behavior tell us about adherence?
In the field of health and healthcare, the TPB has largely been applied to the examination of lifestyle decisions, such as healthy eating.3 However, the theory also has been applied in studies looking at adherence in multiple sclerosis treatment, as considered in the previous article, where TPB can be an important predictor of how patients will behave.4 The TPB also has been used to design behavioral interventions in healthcare. The theory can help construct programs to promote healthy habits,5 and meta-analyses of programs designed around TPB have found that incorporating these additional considerations can lead to positive outcomes.6
Influencing the patient using the Theory of Planned Behavior
The last article in this series discussed the use of the Health Belief Model (HBM) to guide discussions with patients about their understanding of their disease and treatment plans. In healthcare, incorporating the TPB model into HBM helps healthcare providers explore in further detail additional factors that influence patient attitudes and beliefs about their situation.
The HBM does not explicitly address social influences. As an expectancy–value model, the HBM falls short on recognizing the importance of considerations that are not entirely rational. The TPB adds an important social element by taking into account the fact that people are social beings and can have strong reactions to behaviors that are perceived to affect social standing.
The TPB also considers the patient’s ideas regarding perceived control: i.e. whether the patient has control over the disease and its treatment; and beyond decisions about whether the patient thinks their behavior should change, to what degree does the patient feel sufficiently empowered to actually make a behavior change?
The TPB can help providers understand if there are factors that may influence patient behavior that are not addressed by the HBM. To apply the TPB, healthcare providers should consider the following suggestions:
- Ask the patient how difficult he thinks it will be to carry out suggestions and follow the prescription.
- Ask the patient what he thinks might lead to failure.
- Inquire about the degree to which the people close to the patient will either help or hinder behavior changes.
- Discuss the patient’s perception of what other people or society in general might feel about the condition or treatment behaviors.
Questions such as these can help uncover underlying issues with the patient’s perceived control over their behavior, concerns they have about the social impact of their condition, and whether those close to them or society as a whole may pose an impediment to treatment adherence.
Using the TPB: An example
Consider the case of a patient who suffers from vertigo. Having used the Health Belief Model as outlined in the previous article, the provider is confident that the patient has a good grasp of her disease and treatment plan. Using the TPB, the provider now inquires into any concerns the patient may have about her ability to control her behavior and about social norms or influences that might hinder the patient from adhering to the treatment plan. By incorporating the suggestions above, the provider may go beyond the HBM to discover that the patient is concerned she will forget her daily medication and that she feels ashamed of her condition: She thinks her occasional dizziness is a sign of weakness.
From this additional information, the healthcare provider can address the forgetfulness concern by suggesting simple tips on how to remember to take the medication, like associating it with another daily activity, such as breakfast or brushing teeth. The provider can address the feelings of shame by referencing famous and respected political or entertainment figures who also suffer from a similar condition.
These simple measures, based on the additional information uncovered with the TPB model, can have a profound impact on a patient’s attitudes towards her condition, help her adhere to her treatment plans, and improve outcomes.












